Women report experiencing more frequent and intense gut pain compared to men, and now, new research suggests a clear biological reason: the female sex hormone estrogen amplifies pain signals in the gut. The study, conducted on mice and published in Science on December 18, uncovers a previously unknown chain reaction where estrogen increases gut nerve sensitivity, potentially explaining the higher rates of conditions like Irritable Bowel Syndrome (IBS) in women.
The Disparity in Gut Pain: A Long-Standing Question
IBS affects 10–15% of people worldwide, but women are diagnosed up to twice as often as men. Symptoms include chronic pain, bloating, diarrhea, and constipation, all triggered by factors like stress or diet. Despite this clear pattern, the underlying cause of this gender difference has remained unclear — until now.
How Estrogen Amplifies Gut Pain
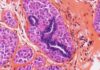
Researchers at the University of California, San Francisco, found that estrogen doesn’t act directly on previously suspected gut cells. Instead, it affects rare L-cells in the gut lining, causing them to produce more OLFR78 receptors. These receptors amplify sensitivity to short-chain fatty acids (byproducts of bacterial digestion), which then trigger the release of a hormone (PYY) that signals pain to the brain.
“We’ve long suspected that female hormones play a role in gut pain, but the exact mechanism was unclear. Our findings show a clear pathway for how estrogen can amplify pain signals,” explains senior study author David Julius.
Removing ovaries in mice reduced gut sensitivity to male levels, while restoring estrogen brought the pain response back to higher levels in females. Experiments using genetically engineered mice lacking estrogen receptors on L-cells confirmed the cells’ critical role.
Implications for Treatment and Understanding
The findings suggest that PYY and OLFR78 could be potential targets for developing new IBS treatments specifically for women. The research also validates the experiences of patients whose symptoms fluctuate with their menstrual cycle or hormone therapy.
Marissa Scavuzzo, an assistant professor at Case Western Reserve University, notes the study’s importance in acknowledging historically overlooked pain differences in women. She also highlights the relevance of these findings to post-menopausal patients and individuals undergoing gender-affirming hormone therapy.
From Mice to Humans: What’s Next?
While promising, the study’s findings require further validation in human clinical trials. Human guts are more complex, with individual variations in lifestyle, genetics, and gut microbiome that can influence hormone-gut interactions. However, this research provides a crucial starting point for understanding why women experience more severe gut pain and developing targeted therapies.
The study also reinforces the potential benefits of low-FODMAP diets, which reduce bacterial sugar intake and may alleviate IBS symptoms by reducing gut fermentation. Overall, this research marks a significant step forward in acknowledging and addressing gender-based differences in chronic pain conditions.